Every country has their own procedure and guideline regarding this pandemic matter, so please refer to your country’s guideline for more details. This is just the summary from WHO and CDC regarding the management and treatment of COVID-19.
Reported illnesses have ranged from mild symptoms to severe illness and death for confirmed coronavirus disease 2019 (COVID-19) cases.
These symptoms may appear 2-14 days after exposure(based on the incubation period of MERS-CoV viruses).
- Fever
- Cough
- Shortness of breath
If you develop emergency warning signsfor COVID-19 get medical attention immediately. Emergency warning signs include*:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face

Management of cases(s) and Contacts
All patients with suspected COVID-19 who have severe acute respiratory infection should be triaged and isolated at the first point of contact with the health care system. Emergency treatment should be started based on disease severity
Screening and Triage
- Mild Illness (81%)
- -Older and/or with comorbidities (e.g. cardiovascular disease & diabetes) should be admitted to a designated unit for close monitoring.
- -(-) comorbidities and other risk factors hospitalization may not be required unless there is concern about rapid deterioration or an inability to promptly return to hospital, but isolation to contain/mitigate virus transmission should be prioritized. All patients cared for outside hospital (i.e. at home or non-traditional settings) should be instructed to manage themselves appropriately according to local/regional public health protocols for home isolation and return to a designated COVID-19 hospital if they get worse.
- -Patients also provided with symptomatic treatment such as antipyretic for fever.
2.Severe Illness (14%)
- –Oxygen therapy and optimized supportive care treatments and safe, rapid referral and admission to a designated hospital ward or intensive care unit according to institutional or national protocols.
3.Critically Ill (5%)
- –Intensive care unit as they mostly require mechanical ventilation
Collection of Specimens for Laboratory Diagnosis and Radiographic Examinations
Blood cultures are collected for bacteria that cause pneumonia and sepsis, ideally before antimicrobial therapy. DO NOT delay antimicrobial therapy to collect blood cultures
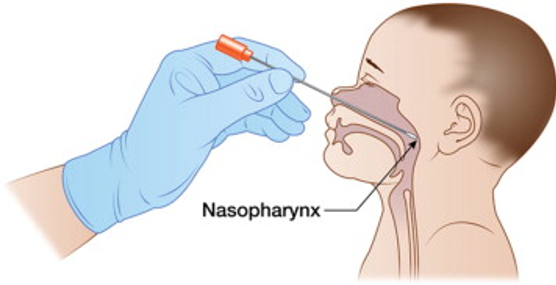
Specimens from the upper respiratory tract (URT; nasopharyngeal and oropharyngeal) AND, where clinical suspicion remains and URT specimens are negative, collect specimens from the lower respiratory tract when readily available (LRT; expectorated sputum, endotracheal aspirate, or bronchoalveolar lavage in ventilated patient) for COVID19 virus testing by RT-PCR and bacterial strains/cultures.
In hospitalized patients with confirmed COVID-19, repeated URT and LRT samples can be collected to demonstrate viral clearance. The frequency of specimen collection will depend on local epidemic characteristics and resources. For hospital discharge, in a clinically recovered patient, two negative tests, at least 24 hours apart, is recommended.
Chest radiographs of patients with COVID-19 typically demonstrate bilateral air-space consolidation, though patients may have unremarkable chest radiographs early in the disease.Chest CT images from patients with COVID-19 typically demonstrate bilateral, peripheral ground glass opacities. Because this chest CT imaging pattern is non-specific and overlaps with other infections, the diagnostic value of chest CT imaging for COVID-19 may be low and dependent upon interpretations from individual radiologists.
Oxygen therapy and Monitoring
- Oxygen therapy will be given immediately to patients with SARI and respiratory distress, hypoxemia or shock and target SpO2 > 94%
- Patients will be closely monitored for signs of clinical deterioration
- Patients with comorbidities will be determined which chronic therapies should be continued and which should be stopped temporarily.
- Fluid management in patients with SARI when there is no evidence of shock

Contacts
- For contacts of a suspected COVID-19 case, at a minimum, health authorities need to encourage respiratory and hand hygiene and may encourage, depending on the epidemiological context and resources available, self-monitoring for symptoms, social distancing, or quarantine.
- For contacts of a laboratory-confirmed COVID-19 case, WHO recommends that such persons be quarantined for 14 days from the last time they were exposed to a COVID-19 patient.










